Deep Vein Thrombosis (DVT) happens when a blood clot forms in a deep vein, most often in the legs. Because these clots can slow or block blood flow, it’s helpful to know the early signs and understand how the condition develops. Many people are surprised to learn that DVT can begin with very subtle symptoms, or sometimes none at all, which is why awareness makes such a difference.
Here in Toronto and throughout Ontario, long hours of sitting during commutes, busy workdays, and reduced movement in the winter months can all influence circulation. With these factors in mind, having a clearer understanding of DVT can help you feel more informed and better prepared to recognize when something may need attention.
Common Signs & Symptoms of a Blood Clot (Deep Vein Thrombosis)
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, most commonly in the leg. Symptoms can develop gradually or appear suddenly, and they don’t always feel severe at first. Because early signs are sometimes subtle, it’s important to know what to watch for, especially if you have risk factors such as prolonged sitting, recent surgery, injury, or circulation issues.
Common signs and symptoms of a blood clot in the leg may include:
- Swelling in one leg (unilateral swelling), usually affecting the calf or thigh rather than both legs
- Warmth in the affected area, which may feel noticeably warmer than the surrounding skin
- Redness or skin discoloration, sometimes appearing slightly purple or darker than usual
- Leg pain, heaviness, or tenderness, often described as a deep ache or cramp, especially when walking or flexing the foot
- Veins that appear firm, hard, or sore to the touch
It’s also important to note that some people experience very mild symptoms, or no noticeable symptoms at all, which is why DVT can sometimes go undetected until complications develop.
Seek Medical Help Immediately
In some cases, a blood clot can break loose and travel to the lungs, causing a pulmonary embolism (PE). This is a medical emergency that requires immediate attention. Seek urgent medical care if you experience any of the following:
- Sudden shortness of breath
- Chest pain or discomfort, especially when breathing deeply
- Coughing up blood
Prompt diagnosis and treatment can be life-saving. If you are unsure whether your symptoms are serious, it is always safer to seek medical advice as soon as possible.
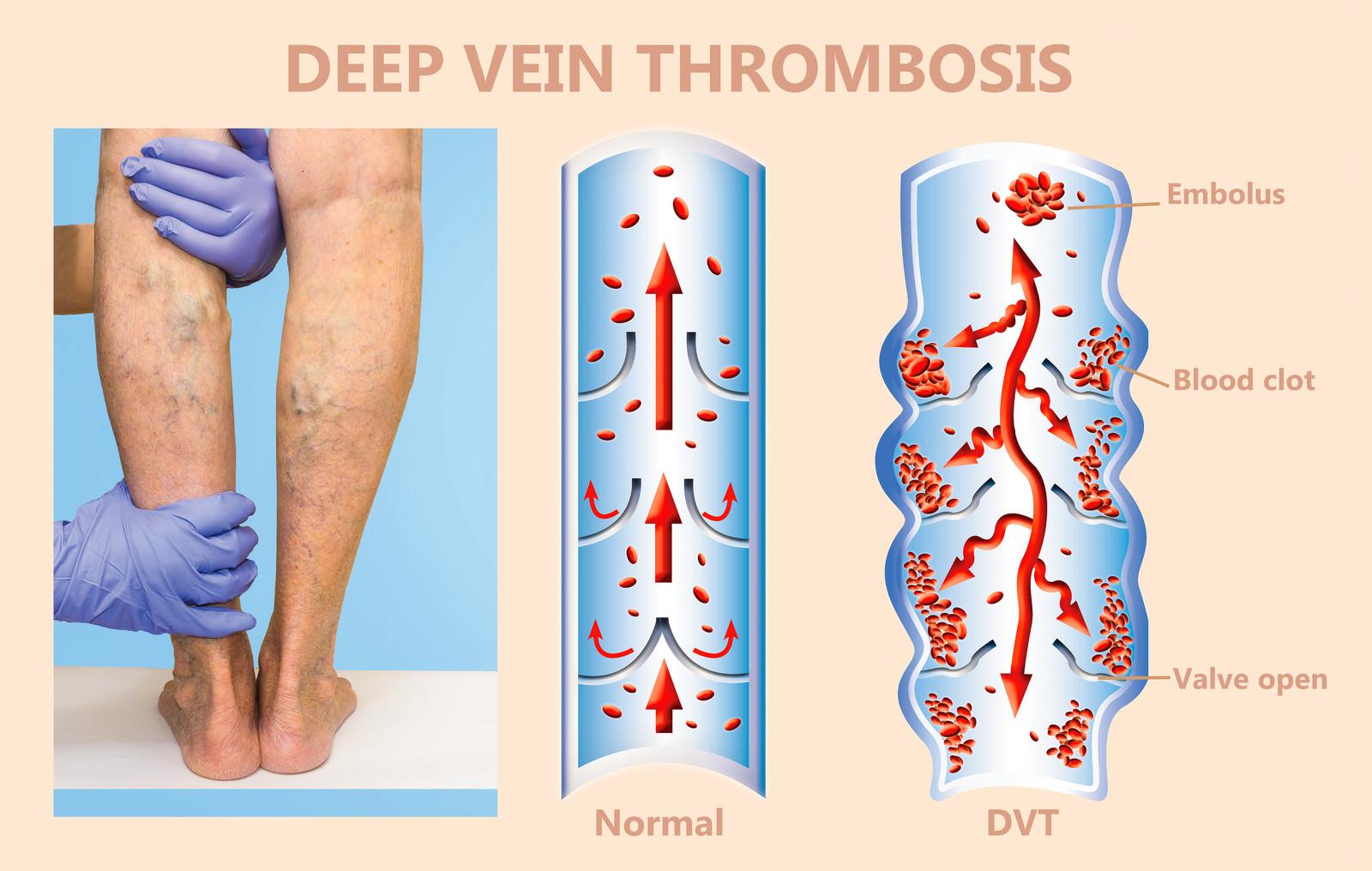
How Deep Vein Thrombosis (DVT) Forms
Deep Vein Thrombosis develops when a blood clot forms in a vein that sits deep within the body, most often in the lower leg or thigh. These veins are responsible for carrying blood back toward the heart, so when a clot appears, it can slow circulation or block it entirely.
DVT is different from clots that form in veins near the surface of the skin. Superficial clots may cause discomfort but are usually less serious. A deep vein clot, however, has the potential to travel or lead to complications if it isn’t recognized and treated promptly.
Blood clots can form for many reasons, slower circulation, injury to the vein, certain medical conditions, or long periods of reduced movement. In some cases, people don’t experience noticeable symptoms at all, which is why knowing the risk factors and early signs can be so helpful.
What Increases the Risk of DVT?
Deep Vein Thrombosis can develop for several reasons, and understanding the most common risk factors can make it easier to recognize when extra caution is needed. Many of these factors influence how well blood moves through the veins or how easily a clot can form.
Some of the most common contributors include:
- Long periods of sitting or inactivity – extended desk work, long car rides, or lengthy flights can slow circulation in the legs.
- Recent surgery or injury – especially procedures involving the legs, hips, or abdomen, which can impact blood flow or temporarily limit movement.
- Age – the risk increases as we get older, particularly over age 60.
- Pregnancy and postpartum changes – natural shifts in blood flow and pressure can raise clotting risk.
- Hormonal birth control or hormone therapy – some medications can affect clotting tendencies.
- Varicose veins or vein disease – conditions that already impact circulation can make clot formation more likely.
- Smoking – affects blood vessels and circulation.
- Obesity – increases pressure in the veins of the lower body.
- Certain medical conditions – including cancer, heart disease, and clotting disorders.
Being aware of these factors doesn’t mean you’ll develop DVT, it simply helps you understand when to pay closer attention to how your legs feel and when symptoms may be worth discussing with a healthcare provider.
Early Warning Signs of Deep Vein Thrombosis
Deep Vein Thrombosis can be easy to overlook in its early stages, especially because symptoms can vary from person to person. Still, there are several changes in the legs that often signal a clot may be forming. Paying attention to these signs can help you seek care sooner and reduce the chance of complications.
Common symptoms include:
- Swelling in one leg, often developing gradually
- Warmth in the calf or thigh, compared to the surrounding skin
- Redness or a change in skin colour over the affected area
- A feeling of tightness or heaviness in the leg
- Pain or tenderness, especially when walking or flexing the foot
- A firm or thickened area along the vein
It’s also possible to have DVT without noticeable symptoms at all, which is why being aware of your risk factors can be just as important as recognizing physical changes.
Some symptoms require immediate medical attention, for example, severe shortness of breath, chest pain, coughing up blood, or a sudden rapid heartbeat. These may indicate that a clot has moved to the lungs, which is a medical emergency.
What to Expect During Diagnosis
If a healthcare provider suspects DVT, the diagnostic process is usually straightforward and designed to give clear answers as quickly as possible. The goal is to confirm whether a clot is present and determine the safest treatment plan.
The most common diagnostic tool is an ultrasound, which uses sound waves to create an image of the veins in your leg. This test is painless, non-invasive, and can usually detect reduced blood flow or the presence of a clot.
A clinician may also:
- Examine the leg for swelling, warmth, tenderness, or colour changes
- Review your medical history and risk factors
- Order a D-dimer blood test, which measures substances released when a clot forms (useful in some cases, but not always required)
If the ultrasound results are unclear or if the clot may be in a harder-to-see location, additional imaging may be recommended. These situations are less common, and your healthcare provider will guide you through the safest next steps.
How Deep Vein Thrombosis Is Treated
Treatment for DVT focuses on preventing the clot from growing, reducing the risk of complications, and supporting healthy circulation as the body heals. Most people begin treatment soon after diagnosis, and many can continue recovery comfortably at home with proper medical guidance.
The most common treatment approaches include:
- Anticoagulant medications (blood thinners)
These medications don’t dissolve the clot, but they help stop it from getting larger and reduce the chance of new clots forming. They’re often taken for several months, depending on your individual situation and risk factors. - Clot-removal procedures
In certain cases, usually when a clot is large, causing significant symptoms, or located in a high-risk area, a doctor may recommend a procedure to break up or remove the clot. This is less common and depends on specific medical circumstances. - Vena cava filters
Very rarely, if someone cannot take anticoagulants, a filter may be placed in a large vein to help prevent clots from traveling to the lungs. This is reserved for special situations. - Supportive measures
Elevating the leg, walking as recommended, and following medical advice on activity levels all help improve circulation. Regular follow-ups ensure the treatment plan is working effectively.
Throughout treatment, most people continue daily life with minimal interruption. The key is early recognition and consistent medical guidance, which help lower the risk of complications and support recovery.
How Compression Can Support DVT Recovery
Compression therapy is often recommended as part of recovery after a Deep Vein Thrombosis, especially once treatment has begun and your healthcare provider confirms it’s safe to use. Graduated compression stockings apply gentle pressure to the legs, helping blood move upward more efficiently and reducing the pooling that can contribute to swelling or discomfort.
Many people find compression helpful for:
- Reducing swelling in the lower legs
- Improving circulation during daily activities
- Easing feelings of heaviness or tightness
- Lowering the risk of post-thrombotic syndrome, a condition that can cause long-term swelling and chronic discomfort after a DVT
A proper fit is important. Stockings that are too tight, too loose, or not the right compression level may not provide the support your legs need. A professional fitting ensures the correct size, pressure, and style, especially if the affected leg is still swollen or tender.
Most individuals describe compression as supportive rather than restrictive when it fits well. It should feel comfortable enough to wear throughout the day and should work alongside your prescribed medical treatment to encourage a healthier recovery.
Tips to Lower the Risk of DVT
While not all cases of Deep Vein Thrombosis can be prevented, simple daily habits can help improve circulation and reduce overall risk. These steps are especially useful during periods of reduced activity, long travel, or colder months when movement naturally decreases.
Some helpful ways to support healthier blood flow include:
- Move regularly throughout the day
Stand, stretch, or take a brief walk every hour if you sit for long periods. Small movements keep blood flowing through the leg veins. - Stay hydrated
Consistent hydration helps blood circulate more easily and supports overall vein health. - Stretch during travel
On long flights or car rides, try ankle circles, calf squeezes, or short walking breaks whenever possible. - Elevate your legs
Raising your legs for a few minutes at the end of the day can ease swelling and improve circulation. - Wear compression during long travel or periods of inactivity
Graduated compression stockings can help guide blood upward and reduce the risk of clot formation when you’re sitting for long stretches. - Maintain regular activity
Walking, light exercise, or gentle indoor movement helps keep leg muscles active and supports healthy blood flow. - Be mindful of other risk factors
Conditions such as varicose veins, past clots, or certain medications may increase risk, discussing these with a healthcare provider can help you create a personalized prevention plan.
Knowing When It’s Time to Talk to a Professional
Paying close attention to changes in your legs can help you decide when it’s time to seek medical guidance. While not every ache or swelling is related to Deep Vein Thrombosis, certain symptoms deserve prompt attention to ensure your safety and comfort.
It’s a good idea to speak with a healthcare provider if you notice:
- Persistent swelling in one leg
- Warmth or redness that doesn’t improve
- A feeling of tightness or heaviness that seems unusual
- Pain in the calf or thigh, especially if it worsens when walking
- Discomfort that appears after long travel, surgery, or inactivity
These signs don’t automatically mean you have DVT, but they do indicate that your body may need extra care. Reaching out early helps rule out serious issues and allows for timely treatment if needed.
If symptoms ever become severe, such as sudden shortness of breath, chest pain, or coughing up blood, seek emergency care immediately, as these can signal a more urgent complication.
Supporting Healthy Circulation
Leg discomfort and swelling shouldn’t be ignored, especially when symptoms are new, persistent, or affect only one leg. Early evaluation and appropriate care play an important role in reducing the risks associated with deep vein thrombosis.
If compression therapy is part of your treatment or prevention plan, Care-Med can help ensure you’re properly fitted and using products that support circulation without unnecessary discomfort. Our team is available to answer questions and provide guidance customized to your situation.
Share This Story, Choose Your Platform!
Table of Contents
- Symptoms and Treatment of DVT (Deep Vein Thrombosis)
- Common Signs & Symptoms of a Blood Clot (Deep Vein Thrombosis)
- How Deep Vein Thrombosis (DVT) Forms
- What Increases the Risk of DVT?
- Early Warning Signs of Deep Vein Thrombosis
- What to Expect During Diagnosis
- How Deep Vein Thrombosis Is Treated
- How Compression Can Support DVT Recovery
- Tips to Lower the Risk of DVT
- Knowing When It’s Time to Talk to a Professional
- Supporting Healthy Circulation
We specialize in orthotics, body braces, and compression wear tailored to your unique needs in Toronto. Reach out to us at info@caremed.care or call 416-782-5353 to book your fitting and consultation.
Experience the difference of customized solutions designed just for you.